The counterintuitive science of SIBO, mast cells, and the probiotic yogurt everyone warns you about
If you've researched L. reuteri yogurt and histamine intolerance, you've probably encountered the same warning everywhere: "L. reuteri produces histamine—avoid it if you're histamine sensitive."
This sounds logical. Histamine causes your symptoms. A bacterium produces histamine. Therefore, avoid the bacterium.
But this advice may be fundamentally wrong. And understanding why it's wrong reveals one of the most misunderstood connections in gut health—one that could explain why you developed histamine intolerance in the first place.
Here's the twist: The histamine L. reuteri produces isn't the same kind that's causing your symptoms. And the root cause of your histamine sensitivity might not be histamine at all. It might be SIBO.
#⚠️ Medical Disclaimer
This article is for educational purposes only and does not constitute medical advice. I am not a physician or healthcare provider.
Before implementing any protocol described here:
- Consult with a licensed healthcare provider
- Disclose all existing conditions and medications
- Obtain professional evaluation specific to your situation
Individual responses to probiotics vary significantly based on genetics, current microbiome, medication interactions, and health status. What works for one person may not work—or may be harmful—for another.
Special caution: Individuals with compromised immune systems, central venous catheters, acute pancreatitis, active infections, or those undergoing cancer treatment should avoid probiotics without explicit specialist authorization.
This article presents an alternative framework based on animal model research and mechanistic understanding. While supported by peer-reviewed research, it has not been validated in large-scale human clinical trials for histamine intolerance specifically.
#The Histamine Most People Miss: H1 vs. H2 Receptor Signaling
To understand why L. reuteri yogurt might help histamine intolerance rather than worsen it, you need to understand something most articles never mention: not all histamine signaling is created equal.
Your body has four types of histamine receptors (H1, H2, H3, H4). When people talk about "histamine intolerance," they're usually describing H1 receptor activation—the pathway responsible for the classic symptoms: flushing, itching, headaches, hives, nasal congestion, anxiety.
But H2 receptor activation does something different. When histamine binds to H2 receptors on intestinal epithelial cells and immune cells, it triggers an anti-inflammatory cascade:
H2R activation → Adenylyl cyclase → ↑cAMP → Protein Kinase A (PKA) → Suppression of pro-inflammatory cytokines (TNF-α, IL-6, IL-1β)
This isn't theoretical speculation. In a landmark 2015 study published in mBio, researchers at Baylor College of Medicine demonstrated that Lactobacillus reuteri 6475—a histamine-producing strain—significantly suppressed colitis in mice through H2 receptor-mediated signaling. When researchers blocked H2 receptors, L. reuteri lost its anti-inflammatory effects. When they blocked H1 receptors? Nothing changed—L. reuteri continued suppressing inflammation.
The implication is profound: L. reuteri appears to produce histamine specifically to activate anti-inflammatory H2R pathways, not pro-inflammatory H1R pathways.
#"Histamine Intolerance Is Just SIBO"

In his April 2025 article, Dr. William Davis made a provocative but research-supported statement that reframes the entire conversation:
"Histamine intolerance: It's just SIBO."
This doesn't mean they're identical conditions. It means that for many people, the root cause of histamine sensitivity is an underlying small intestinal bacterial overgrowth—and until you address the SIBO, you're just managing symptoms while the underlying problem persists.
If you're new to the SIBO concept, I've covered how SIBO relates to fermented foods in detail—including what's safe and what's not during the healing process.
Here's the mechanism:
#Where Your Histamine Actually Comes From
When you have SIBO, your small intestine becomes colonized by bacteria that don't belong there—species like E. coli, Klebsiella, Salmonella, Enterococcus, and others. These pathogenic bacteria do three things that create a perfect storm for histamine intolerance:

-
They produce histamine indiscriminately. Unlike L. reuteri's targeted H2R signaling, SIBO bacteria flood your system with histamine as a metabolic byproduct.
-
They produce lipopolysaccharide (LPS). This bacterial endotoxin directly activates mast cells, triggering massive histamine release from your own cells—on top of the histamine the bacteria are producing.
-
They crowd out histamine-metabolizing bacteria. Your gut normally contains bacteria that help break down histamine. When SIBO takes over, these beneficial species are outnumbered and outcompeted.
Additionally, the chronic inflammation from SIBO damages your intestinal lining and reduces production of diamine oxidase (DAO)—the enzyme responsible for breaking down histamine locally in your gut.
The result: More histamine production + less histamine breakdown = histamine intolerance.
The problem isn't that you're eating histamine-containing foods. The problem is that your gut has lost its ability to manage normal histamine levels.
#The Counterintuitive Healing Mechanism

If your histamine sensitivity stems from SIBO-driven dysbiosis, here's what the research suggests may happen when you introduce L. reuteri yogurt:
#Phase 1: The Adjustment Period (Days 1-7)
When you introduce L. reuteri into an inflamed, dysbiotic small intestine:
- The existing pathogenic bacteria may respond with increased LPS production
- Your already-sensitized mast cells may react to this microbial shift
- You may experience temporary symptoms: headaches, brain fog, flushing, bloating, sleep disruption
This temporary response is sometimes called a "die-off reaction"—more accurately described as microbial ecosystem stress. Your dysbiotic microbiota is being challenged.
#Phase 2: The Rebalancing (Weeks 2-4)
As L. reuteri establishes itself and activates H2R-mediated anti-inflammatory signaling:
- Pro-inflammatory cytokine production begins declining
- Intestinal inflammation starts resolving
- DAO production may begin recovering as your gut lining heals
- Mast cell reactivity may start normalizing
#Phase 3: The Resolution (Weeks 4-12)
As SIBO resolves and microbial balance returns:
- Histamine production from pathogenic bacteria decreases
- Histamine metabolism capacity increases
- Foods that previously triggered symptoms may become tolerable
The paradox completes: The histamine-producing probiotic helps resolve histamine intolerance by addressing the underlying dysbiosis that caused it.

#Critical: Not All L. Reuteri Strains Are Equal
Before you rush to make L. reuteri yogurt, you need to understand something important: different L. reuteri strains have dramatically different histamine-producing capabilities.
| Strain | Histamine Production | Notes |
|---|---|---|
| L. reuteri 6475 (ATCC PTA 6475) | YES - High | Contains complete hdc gene cluster; anti-inflammatory via H2R |
| L. reuteri DSM 17938 | NO | Lacks hdc genes; does not produce histamine |
| L. reuteri NCIMB 30242 | NO | Different strain; used for cholesterol management |

The anti-inflammatory H2R signaling mechanism described in this article only applies to histamine-producing strains like L. reuteri 6475. The DSM 17938 strain (commonly found in infant probiotics and some commercial products) does NOT produce histamine and operates through different mechanisms.
If you're specifically seeking the H2R-mediated anti-inflammatory effects, verify your product contains the 6475 strain or another histamine-producing strain with the hdc gene cluster. (Good news: BioGaia Gastrus contains both strains, making it an ideal starter for the yogurt protocol.)
For my complete guide to making L. reuteri yogurt with the correct strains, check out The Yogurt Awakening: Why Dr. Davis's L. Reuteri Recipe Is a Game-Changer for Gut Health.
#When to Address SIBO First vs. When to Proceed with L. Reuteri
This is the critical practical question, and the answer depends on your severity—with professional guidance.
#Severe Histamine Sensitivity: Consider a Two-Phase Approach
If you experience severe symptoms—extreme headaches, significant skin reactions, major sleep disruption, or suspected mast cell activation—you may benefit from addressing the acute SIBO bacterial burden first.
Phase 1: Microbial Suppression (2-4 weeks)
Work with a healthcare provider on herbal antimicrobial protocols. Two regimens have clinical evidence for efficacy against SIBO:
- CandiBactin-AR + CandiBactin-BR
- FC-Cidal + Dysbiocide (with NAC and curcumin)
A 2014 retrospective study from Johns Hopkins showed these herbal protocols were at least as effective as rifaximin for SIBO eradication.
Phase 2: Microbial Restoration (4+ weeks)
Once the acute bacterial burden is reduced, introduce L. reuteri yogurt using the gradual protocol below.
#Moderate Histamine Sensitivity: Concurrent Approach May Work
If you have moderate symptoms—occasional headaches, mild skin reactions, some sleep disruption—you might tolerate introducing small amounts of L. reuteri alongside herbal antimicrobial support. The antimicrobials suppress pathogenic bacteria and LPS production while L. reuteri begins H2R-mediated signaling.
Start with extremely small amounts (1-2 teaspoons daily). If you experience significant flares, pause the yogurt and focus on antimicrobials for 1-2 weeks before retrying.
#Mild Histamine Sensitivity
If you have mild symptoms or suspected subclinical SIBO, you may be able to proceed directly with L. reuteri yogurt using the gradual introduction protocol.
#The Start-Low Protocol: Gradual Introduction for Histamine-Sensitive Individuals
The conventional approach—taking a full dose immediately—can overwhelm sensitive individuals. This gradual protocol may help:
#Week 1: Microdose Introduction
- Days 1-3: ¼ teaspoon once daily, with food
- Days 4-7: ½ teaspoon once daily, with food
- Track: GI symptoms, headaches, flushing, brain fog, sleep quality
- Expected: Some bloating or gas; should resolve within 3-5 days
- Red flag: Severe headaches or significant symptoms lasting more than 2-3 days → pause and consult healthcare provider
#Weeks 2-3: Gradual Escalation
- Week 2: 1 teaspoon once daily
- Week 3: 1 teaspoon twice daily (morning and evening)
- Expected: Continued minor adjustment symptoms with gradual baseline improvement
#Week 4+: Full Dose Integration
- Target dose: 1-2 tablespoons daily, divided between morning and evening
- Timeline: Continue for 8-12 weeks minimum to allow microbiota rebalancing
#If You Experience a Flare
Don't just stop. Consult with your healthcare provider about:
- Pausing for 3-5 days (return to last tolerated dose)
- Supporting mast cells: Quercetin, luteolin (dosing per provider guidance)
- Reducing histamine load: Strict low-histamine eating for 3-5 days
- Minimizing stressors: Reduce stress, optimize sleep, avoid vigorous exercise
- Restarting more slowly: Wait 7-10 days between dose increases instead of 3-4 days
Most people need only 1-2 pause-restart cycles to find their trajectory.
#Making L. Reuteri Yogurt: Quick Equipment Notes

The 36-hour fermentation required for L. reuteri yogurt needs precise temperature control at 100-106°F—well below what standard yogurt makers maintain.
The easiest method is using a sous vide immersion circulator like the Anova Precision Cooker. I've compared all three Anova models for fermentation work—any will handle the job beautifully, but the Precision Cooker 3.0 hits the sweet spot of features and price.
For the complete SIBO yogurt recipe—including the three-strain combination with L. gasseri and B. coagulans that many find even more effective—check out my Dr. Davis SIBO Yogurt Recipe guide.
#Companion Strategies: Creating a Supportive Environment
L. reuteri yogurt is one piece of a comprehensive approach. Consider these supporting strategies under professional guidance:
#Temporary Low-Histamine Eating Pattern (Weeks 1-4)
Prioritize:
- Fresh meat/fish (cooked same day)
- Fresh vegetables (not fermented)
- Fresh fruit (not overripe)
- Rice, potatoes, eggs
- Ghee, coconut oil, olive oil
Minimize:
- Aged cheeses, cured meats
- Fermented vegetables (sauerkraut, kimchi)
- Alcohol, long-stored leftovers
- Tomato sauce, spinach, avocado, chocolate

As sensitivity improves (typically by week 6-8), you can gradually reintroduce previously problematic foods. For a deeper dive on navigating fermented foods during gut healing, see my Complete Guide to Low-FODMAP Fermented Foods That Actually Work.
#DAO Support (Early Phase)

DAO enzyme supplements may help bridge the gap while your natural production recovers. Work with a provider on appropriate dosing—this addresses symptoms, not root cause.
#Mast Cell Support
Common supportive nutrients (consult provider on dosing):
- Quercetin: Natural H1 blocker, mast cell stabilizer
- Magnesium glycinate: Mast cell support, DAO cofactor
- Vitamin C: DAO cofactor, anti-inflammatory
- B6: HNMT enzyme cofactor
#Sleep Optimization

Histamine is metabolized primarily during deep sleep. Target 8-9 hours in a dark, cool room (64-68°F).
#Stress Management
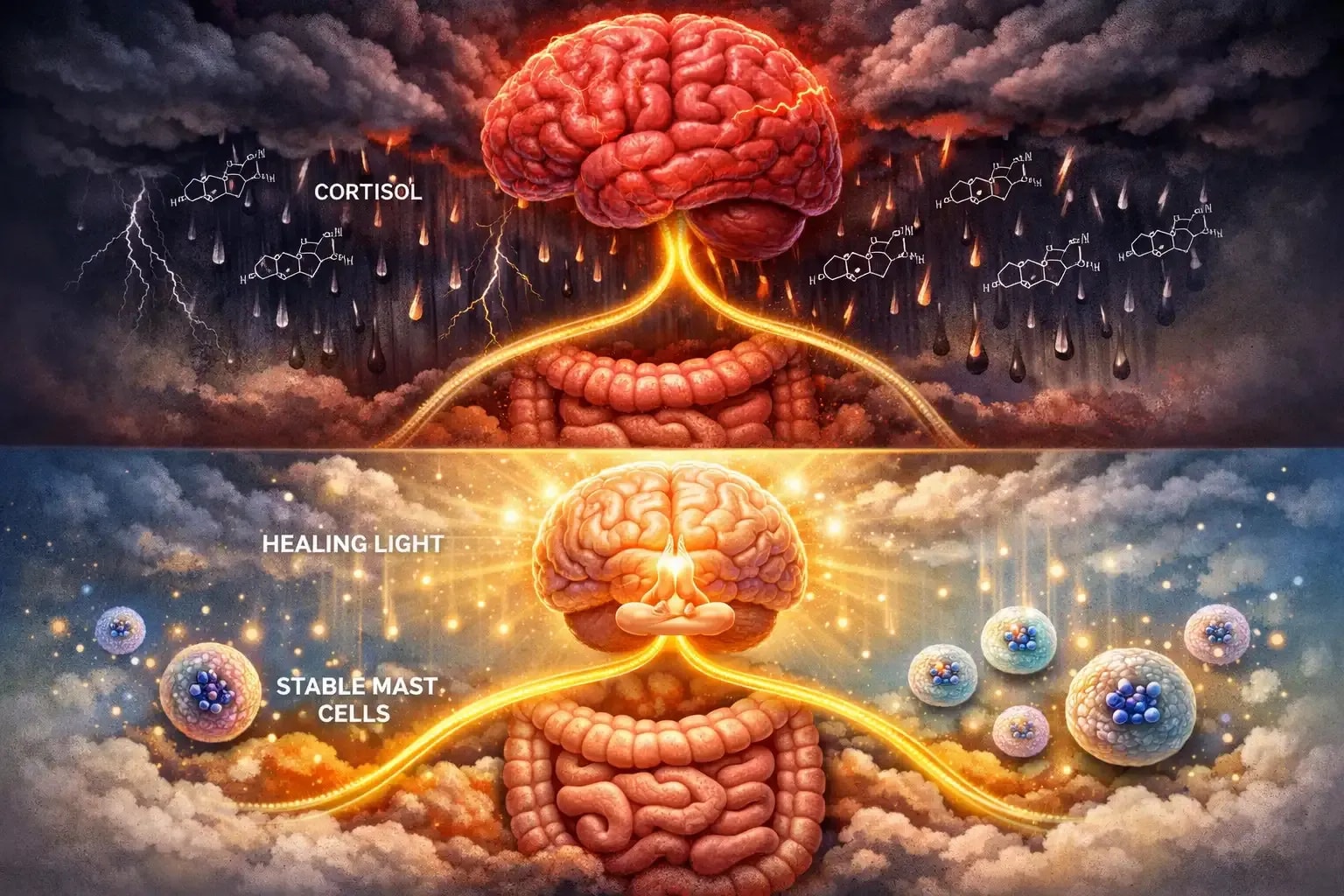
Chronic stress elevates cortisol, which may suppress DAO production and activate mast cells. Daily meditation, yoga, or breathwork isn't optional—it's part of the protocol.
#The Research Foundation
This framework draws on peer-reviewed research, though human clinical trials specifically for histamine intolerance remain limited:
#Key Animal Model Studies
Gao et al. (2015) - mBio
"Histamine H2 Receptor-Mediated Suppression of Intestinal Inflammation by Probiotic Lactobacillus reuteri"
- Demonstrated that hdc+ (histamine-producing) L. reuteri suppressed colitis in mice
- Effect depended on H2R signaling; blocked by H2R antagonists
- H1R blockade had no effect on anti-inflammatory activity
- Full text: PMC4701830 | PMID: 26670383
Thomas et al. (2012) - PLoS One
"Histamine Derived from Probiotic Lactobacillus reuteri Suppresses TNF via Modulation of PKA and ERK Signaling"
- Identified histamine as the TNF-inhibitory compound produced by L. reuteri 6475
- Demonstrated H2R-dependent mechanism via cAMP/PKA pathway
- Full text: PMC3285189 | PMID: 22384111
Hemarajata et al. (2013) - Journal of Bacteriology
"Lactobacillus reuteri-specific immunoregulatory gene rsiR modulates histamine production"
- Characterized the rsiR gene essential for TNF suppression
- Linked histamine production to anti-inflammatory effects
- Full text: PMC3889603 | PMID: 24123819
Gao et al. (2017) - American Journal of Pathology
"Gut Microbe–Mediated Suppression of Inflammation-Associated Colon Carcinogenesis by Luminal Histamine Production"
- hdc+ L. reuteri reduced colon tumors in mice
- HDC-deficient mutants showed no protective effect
- Full text: PMC5809336 | PMID: 28917668
Shi et al. (2019) - American Journal of Physiology
"Distinct roles of histamine H1- and H2-receptor signaling pathways in inflammation-associated colonic tumorigenesis"
- Clarified opposing roles of H1R (pro-inflammatory) vs. H2R (anti-inflammatory) signaling
- Full text: PMC6383385 | PMID: 30462522
#Clinical Framework
Dr. William Davis (April 2025)
"Histamine intolerance: It's just SIBO"
- Synthesizes clinical observations on SIBO-histamine connection
- Read article
Chedid et al. (2014) - Global Advances in Health and Medicine
"Herbal Therapy Is Equivalent to Rifaximin for the Treatment of Small Intestinal Bacterial Overgrowth"
- Johns Hopkins retrospective analysis showing herbal protocols equivalent to antibiotics for SIBO
- Supports herbal antimicrobial approach
- Full text: PMC4030608 | PMID: 24891990
#The Bigger Picture: Root Cause vs. Symptom Management
Here's the uncomfortable truth about conventional histamine intolerance advice:
"Avoid aged cheese, fermented foods, and histamine-producing probiotics" addresses symptoms while ignoring root cause.
Dr. Davis makes the analogy: Avoiding histamine-containing foods while ignoring SIBO is like taking antacids for acid reflux while continuing to smoke. You might feel temporarily better, but the underlying pathology persists—and potentially worsens.

The consequences of untreated SIBO extend far beyond histamine symptoms:
- Increased visceral fat accumulation
- Insulin resistance and metabolic dysfunction
- Cardiovascular risk factors
- Neurological symptoms (anxiety, depression, brain fog)
- Skin conditions (rosacea, psoriasis, eczema)
- Autoimmune conditions
And food avoidance itself can perpetuate dysbiosis. As you eliminate fermented foods and fiber-rich vegetables, you reduce microbial diversity and short-chain fatty acid production—potentially worsening the very conditions driving your sensitivity.
The path forward isn't permanent restriction. It's restoration of a healthy, diverse microbiota that metabolizes histamine efficiently. And L. reuteri—despite producing histamine—appears to be a keystone species in that restoration.
#Practical Next Steps
#Step 1: Confirm Underlying Conditions
- SIBO testing: Lactulose or glucose breath test with healthcare provider
- Histamine sensitivity evaluation: Professional assessment to rule out other conditions
- Microbiome status: Stool testing if indicated
#Step 2: Choose Your Approach (With Professional Guidance)
| Severity | Recommended Approach |
|---|---|
| Severe | Two-phase: Herbal antimicrobials first (2-4 weeks), then gradual L. reuteri introduction |
| Moderate | Concurrent: Small L. reuteri amounts alongside antimicrobial support |
| Mild | Direct: Start-low L. reuteri protocol with mast cell support |
#Step 3: Execute the Protocol
- Follow gradual introduction schedule
- Track symptoms daily
- Adjust based on individual response
- Target: 1-2 tablespoons daily by Week 4-6
#Step 4: Long-Term Maintenance
- Continue L. reuteri yogurt as part of regular routine
- Gradually reintroduce previously problematic foods
- Maintain sleep quality, stress management, whole-foods diet
- Consider periodic gut health assessment
#The Bottom Line
You may not have a histamine intolerance. You may have a dysbiotic, inflamed small intestine that has lost its capacity to metabolize histamine.
L. reuteri yogurt—despite producing histamine—is one of the most researched tools for addressing this root cause. The temporary symptoms some people experience aren't necessarily a sign of harm. They may be evidence that the microbial ecosystem is beginning to rebalance.
When you understand the H2 receptor mechanism, the role of SIBO-derived histamine versus L. reuteri-derived histamine, and the inflammatory cascade driven by pathogenic bacteria and LPS, the logic becomes consistent:
The solution to histamine intolerance might not be lifelong avoidance. It might be restoration of a healthy microbiota that metabolizes histamine efficiently—and L. reuteri appears to be a key player in that restoration.
This is why people who work with healthcare providers, stay disciplined with gradual introduction, and support their healing with mast cell stabilizers, DAO cofactors, and stress management often report significant improvement within 8-12 weeks.
Your gut wants to heal. Your microbiota wants to thrive. Your mast cells want to stabilize. The question is whether you'll address the root cause—or spend years avoiding cheese.

This article synthesizes peer-reviewed research and clinical perspectives. All recommendations require individual assessment and implementation under qualified healthcare provider guidance. Individual results vary significantly based on genetics, current microbiota composition, SIBO severity, and overall health status.




